Weight loss Management Program
Endovascular Bariatric Procedure
Obesity is a well-known major public health concern that causes significant morbidity and mortality with severe effects on the healthcare system and its financial status. Classic treatment options for obesity include lifestyle interventions, pharmacotherapy, and bariatric surgery. However, there is a treatment gap for patients in whom lifestyle modifications were not sufficient or satisfactory, and yet bariatric surgery is not a suitable option. Bariatric artery embolization (BAE) is a novel, minimally invasive, image-guided endovascular procedure that induces weight loss by reducing the production of appetite-mediating hormones following transarterial embolization of the gastric fundus. Recent evidence has shown that BAE is safe and effective in inducing clinically significant weight.
What is Endovascular GAE Procedure
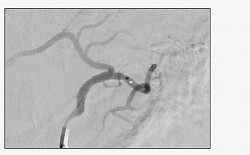
What is left gastric artery embolisation?
Left gastric artery embolisation (LGAE) is a minimally invasive procedure used to treat certain stomach and upper gastrointestinal tract conditions. It involves blocking or reducing blood flow to the left gastric artery, a branch of the celiac artery supplying the stomach. This procedure is usually performed by an interventional radiologist or gastroenterologist.
Main uses of LGAE
Treating bleeding ulcers: LGAE can control severe bleeding from stomach ulcers that do not respond to medical or endoscopic treatments.
Treating obesity: LGAE has been explored as a treatment for obesity. By reducing blood flow to the fundus (upper stomach), it may decrease appetite and food intake, promoting weight loss.
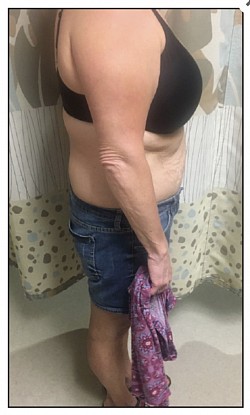
Who is the ideal candidate?
Ideal candidates for LGAE are individuals with obesity who meet certain criteria, including:
- BMI between 35 and 50
- Weight under 150 kg
- Generally fit and well without significant co-morbidities such as diabetes, hypertension, or heart disease
Who may not be suitable for LGAE?
Some factors may exclude individuals from LGAE, including:
- Unsuitable stomach vascular anatomy
- Active H. pylori infection or previous peptic ulcer
- History of bariatric surgery
- Allergy to contrast agents
- Known aorta, renal, or vascular disease
- Previous cancer
- History of radiotherapy in the abdominal area
- Pregnancy
- History of upper or lower gastrointestinal bleeding
- Inability to lie supine during the procedure
The decision to proceed with LGAE should be made with a qualified healthcare provider who will assess medical history and overall health to determine suitability. Up-to-date medical advice is essential for personalised care.
Duration of the procedure
LGAE usually takes about 45 minutes and is performed under sedation. It is minimally invasive, and patients often go home the same day after observation to monitor for immediate complications.
Primary risks involved
LGAE is generally safe but carries some risks, including:
- Gastric erosions causing irritation or discomfort
- Vomiting and abdominal pain that are usually self-limiting
Patient Guide to Procedure
Before Your Procedure
Pre-procedure instructions:
You will be given specific instructions on what to eat and drink in the days leading up to the procedure, including fasting guidelines.
Medical history:
Your doctor will assess your overall health and medical history to ensure you are a good candidate for the procedure.
Anesthesia:
You will be under conscious sedation during the procedure.
Informed consent:
You will be asked to sign an informed consent form after a detailed explanation of the procedure, benefits, and potential risks.
During the Procedure
Minimally invasive: LGAE is performed using a catheter inserted into a blood vessel, often in the groin, and guided to the left gastric artery under Floroscope guidance. Occlusion: The artery is blocked using a material that prevents blood flow.
After Your Procedure
Hospital stay: You will typically be monitored in the hospital 12 hours or 1 day.
Pain management: Pain medication will be prescribed to manage any discomfort.
Diet: You will be instructed on a gradual return to your regular diet, starting with liquids and then solids.
Follow-up appointments: Regular checkups are necessary to monitor weight loss, assess complications, and make any necessary adjustments to your care. Lifestyle changes: LGAE is often used in conjunction with lifestyle changes like dietary adjustments and exercise to promote long-term weight management.